How to Avoid Dehydration in Elderly People: Red Flags and Real-Life Remedies
Learn how to prevent dehydration in elderly people. Discover early warning signs, risk factors, and practical hydration strategies for seniors and caregivers.

One of the health challenges affecting older adults that are considered to be common and dangerous, but are not frequently noticed, is dehydration, which leads to major health complications only in severe cases. Aging causes the individual to lose the feeling of thirst, their kidneys become ineffective and their body becomes less efficient when conserving fluids. Combine medications, underlying conditions, and reduced mobility, and dehydration will turn into a silent killer.
It is much more than just starting to drink more water and preventing dehydration in old age, but rather knowing how the body in old age alters and developing habits, environments and routines to ensure that hydration is easy and routine.
The Reason Behind Dehydration Predominance Among the Elderly
Human body consists of nearly 60 percent water, whereas as we age, the percentage of water in the human body also reduces with age. The seniors usually possess less body fat, which has very little water, and more of the muscles, which store water. Consequently, there is a reduced amount of reserve water when they begin to be dehydrated.
To make the matters worse, the thirst mechanism does decline with time. Most of the elderly people just fail to get thirsty even when the body requires fluids. The part of the brain that controls thirst hypothalamus becomes less sensitive to thirst as a person ages thus seniors can easily forget their water requirements.
Kidneys are also rendered ineffective that is, they are slow in filtering blood and concentrating urine. This results in increased loss of fluids without excessive sweating and activities. Some drugs, like blood pressure diuretics, laxatives, or heart conditions, raise the amount of urine or influence electrolyte levels, which further puts the risk at risk.
Moreover, chronic conditions such as diabetes, Parkinson, or Alzheimer may disrupt the fluid balance and make the elderly unable to take water on their own or to remember about it. Others can even consciously stop consuming water to save on trips to bathrooms or urinating at night.
⚠️ Key Risk Factors
- Reduced body water percentage with age
- Diminished thirst mechanism
- Less efficient kidney function
- Medication side effects (diuretics, laxatives)
- Chronic conditions (diabetes, Parkinson's, Alzheimer's)
- Fear of frequent bathroom trips
The Symptoms of Dehydration: Early and Late Warning Signals
Early detection of the symptoms is one of the greatest difficulties in preventing dehydration in the elderly. The typical symptoms (including thirst) do not manifest themselves in older adults until dehydration is severe.
Early signs include:
- Dry mouth, lips, or tongue
- Headaches or mild dizziness
- Fatigue or sluggishness
- Fewer urination or reddish urine
- Constipation or dry skin
With the increase of dehydration, more serious symptoms can appear, including:
- Disorientation, confusion or irritation
- Increased breathing rate or heart rate
- Low standing blood pressure
- Muscle cramps or weakness
- Loss of consciousness or sleepiness
Dehydration in the elderly may even imitate or exacerbate other conditions such as dementia or urinary tract infections, which are thus admitted to hospital unnecessarily. Caregivers/family members should be educated to watch out to the slightest variations in alertness, balance, or mood - this can be an early indication.
🚨 Warning Signs to Watch For
Early Stage:
- Dry mouth, lips, or tongue
- Headaches or dizziness
- Fatigue or sluggishness
- Dark or infrequent urine
- Constipation or dry skin
Severe Stage:
- Confusion or disorientation
- Rapid breathing or heart rate
- Low blood pressure
- Muscle cramps or weakness
- Loss of consciousness
Risk-Increasing Environment and Lifestyle Factors
However, although a large role is taken by biology, the environment and lifestyle of an elderly also influence it equally. The trigger of hot weather is obvious, as it is not an exception and older bodies that are not very efficient at cooling down may not sweat enough to get the temperatures back to normal. Cold weather is also dangerous: in winter, the elderly drink less due to the fact that they do not feel hot or thirsty, and indoor heating may dry the air, contributing to the loss of water through the skin and breathing.
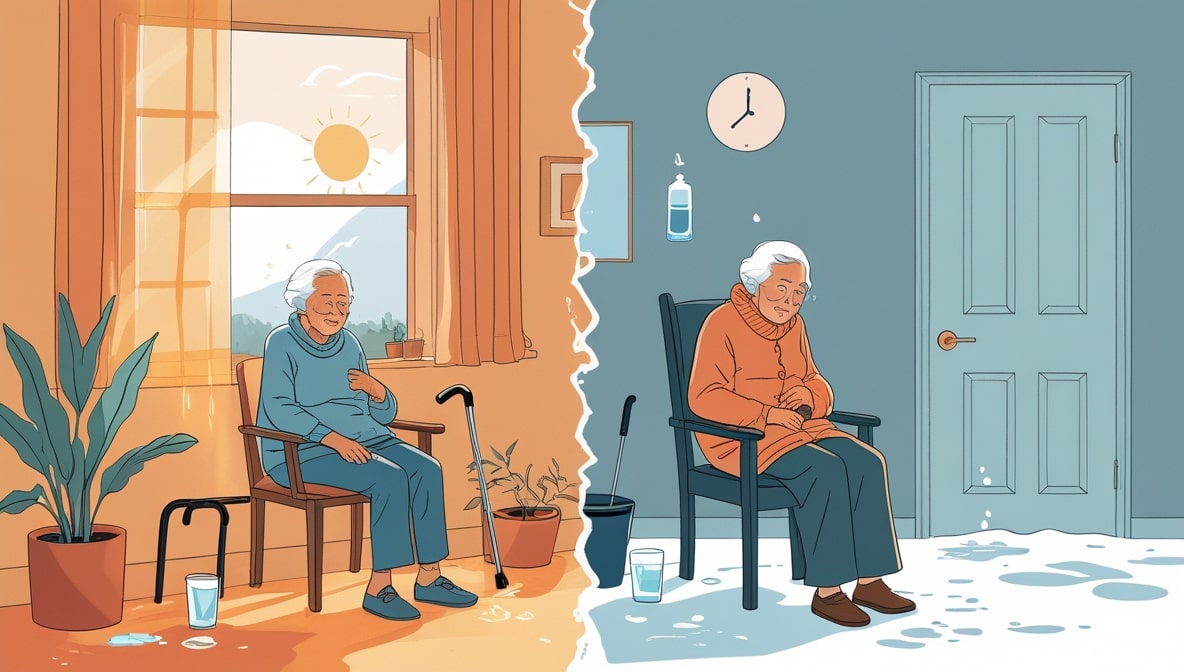
The situation in which one lives is also important. The elderly in assisted living homes or nursing homes can become dependent on staff and fail to hydrate or can have mobility problems to get to the kitchen. Arthritic elderly people with tremors or with a poor grip may have physical difficulties holding a glass or opening a bottle.
There are also psychological causes. Most elders are scared of incontinence and therefore they deliberately reduce on the amount of fluid they consume, to prevent accidents or nocturnal visits to the washrooms. It is, unfortunately, a short-term choice that may boost the risk of dehydration and, in fact, deteriorate the state of urinary health in the long-term.
Useful Dehydration Prevention Strategies
The prevention of dehydration is not about forcing oneself to drink water but about establishing habits, cues, and conditions, which enable people to act hydrated.
The initial one is to establish a hydration schedule. The elderly are also expected to take water periodically during the day as opposed to the timing when they feel thirsty. Adequate hydration occurs with the intake of a full-glass of water upon wakening, with each meal, mid-afternoon and bedtime (assuming tolerance) and hydration is distributed evenly in the body and it helps the kidneys in their work.
Fluids do not necessarily have to be simple water. Most of the elderly do not like its flavor and thus it is better to add variety. Drinking can be made more interesting with the help of herbal teas, flavored waters, diluted fruit juice or milk. Even the hydrating foods contribute to it - soups, yogurt, cucumbers, tomatoes, oranges, and melons are good sources of water.
Caregivers are advised to have water readily available to persons with mobility problems; bedside tables, to their favorite chairs or always within reach. Drinks can be served in lightweight bottles, in spillproof cups or with a straw, so that those with insufficient hand strength can be able to drink.
A system that reminds of hydration can be particularly helpful. It can be as easy as setting an alarm on a phone or watch or writing the times on a water bottle (such as "9 AM," 12 PM, 3 PM) to keep track of the progress made each day.
💡 Prevention Tips
Schedule & Routine:
- Drink water at set times (waking, meals, bedtime)
- Set phone or watch reminders
- Use time-marked water bottles
- Make hydration part of daily routine
Variety & Accessibility:
- Herbal teas, flavored waters, diluted juices
- Water-rich foods (soups, yogurt, fruits)
- Lightweight, spill-proof cups
- Place water within easy reach
Fluid Balance in the Elderly
The following is an example of a basic hydration plan that can be used as a daily model:
📅 Daily Hydration Schedule
- Morning: Morning glass of water after waking up to replenish the lost fluids.
- Breakfast: One glass of food containing food to promote digestion.
- Mid-morning: Flavoured water or herbal tea.
- Lunch: One or two glasses of water or milk.
- Afternoon: A drink and a snack (fruit, yogurt, or soup) that quenches the thirst.
- Dinner: 1 glass water or juice.
- Evening: Before going to bed, water, a little, though safe and comfortable.
This will be approximated to six to eight glasses per day though the specific amount must be determined by the size of the individual, his/her diet, the level of activity and medical conditions.
The Family and the Role of Caregivers
Caregivers can make sure the seniors are well hydrated particularly those with cognitive or mobility issues. Motivation and check-ups get one far. As an illustration, the caregivers could provide beverages instead of posing a question on whether or not a person would like water. It is much better to say Here's some water, have a little of that.

In nursing homes or assisted living facilities, hydration must be included in the everyday nursing care. Staff will have the ability to monitor fluid intake with the help of checklists and make sure seniors get a drink between meals, rather than in the middle of them. To create a social and enjoyable experience, families visiting loved ones will carry hydrating snacks such as smoothies, fruit cups or low-sugar drinks.
Establishing social hydration habits - including tea time with friends/family - are useful in making hydration enjoyable instead of medicinal. Such psychological change tends to give rise to increased consistency.
👨👩👧👦 Caregiver Strategies
- Offer beverages directly instead of asking
- Use checklists to monitor fluid intake
- Provide drinks between meals
- Bring hydrating snacks during visits (smoothies, fruit cups)
- Create social hydration times (tea time with family/friends)
- Make hydration enjoyable, not medicinal
Medical Conditions and Hydration
Some of the medical issues demand more accommodation of hydration. The elderly having heart diseases or kidney issues might be required to control the amount of fluids they take since excess of water is as useless as water scarcity. In this situation, the dietitians or doctors should give certain advice.
Elderly people having dementia or Alzheimer disease might forget to drink at all. Caregivers can make hydration a part of routine routines e.g. drinking water prior to watching television or after cleaning the teeth. Reminders can also be in the form of visual cues such as the use of bright colored cups or pitchers.
Electrolyte balance is particularly essential to those on diuretics or other medications that lead to fluid loss. When the sodium and potassium levels need to be maintained, adding electrolyte-rich drinks (such as coconut water or oral rehydration solution) at least once a day could be useful.
🏥 Special Considerations
Heart/Kidney Conditions:
- May need fluid restrictions
- Consult with doctor or dietitian
- Balance hydration carefully
Dementia/Alzheimer's:
- Link hydration to routines
- Use visual cues (bright cups)
- Regular reminders
When to Seek Medical Help
In case of severe dehydration, then it must be addressed. The signs that include extreme fatigue, confusion, very dark urine, irregular heartbeat, low blood pressure or failing to hold down fluids are an indication of a medical emergency. In this situation, intravenous (IV) fluids might be required to bring this back to balance.
Physicians can also assist in identifying whether frequent cases of dehydration are associated with drug side effects, deterioration of kidney, or some other underlying problem.
🚑 Emergency Warning Signs: Seek Immediate Medical Help
- Extreme fatigue or confusion
- Very dark urine
- Irregular heartbeat
- Low blood pressure
- Unable to hold down fluids
- Loss of consciousness
These symptoms require immediate medical attention and may need IV fluids.
Conclusion
It is not necessarily only a matter of physical health that is associated with preventing dehydration in seniors, but rather saving energy, resilience, and clarity of mind. Hydration influences all body organs including the brain, heart, and the skin.
The risk can be drastically reduced with the help of simple, regular actions, such as available drinks, reminders, alternatives that are both delicious and healthy, and the support of the caregivers. The idea is to make hydration easy and enjoyable whether at home or in assisted living.
By keeping hydrated, the seniors do not just feel better, they feel sharper, easily movable and live longer healthy lives.
Calculate Optimal Hydration for Seniors
Understanding individual hydration needs is crucial for preventing dehydration in elderly people. Our calculator takes into account age-related changes, medication effects, and health conditions to provide safe, personalized recommendations.
Use our senior hydration calculator to get age-appropriate water intake recommendations that help prevent dehydration while avoiding fluid overload, especially important for seniors with heart or kidney conditions.